Vietnam Emergency Protocols for Groups | Corporate Planning
Reading time: 32-40 min Category: vietnam-dmc-operations-and-planning Keyword focus: Vietnam emergency protocols for tour groups Last updated: 2026 Corporate duty of care in Vietnam is not about having a list of hospitals. It is about proving you can locate travelers, activate medical response fast, control costs, and produce an audit-ready incident record if something happens. This guide translates Vietnam emergency realities into a planner-ready protocol for corporate groups (MICE, incentives, and bleisure add-ons). It is designed to be forwarded to internal stakeholders (HR, procurement, security) or attached as an appendix in an RFP response. For related on-the-ground risk controls, also reference our traffic and protocol risks playbook and Hanoi routing playbook. Scope: Medical emergencies, hospital access, emergency contacts, escalation, documentation, and cost-control workflows for groups. For corporate travel managers, Vietnam is operationally manageable when emergency response is planned with realistic assumptions and documented execution controls. Most failures are not medical - they are process failures: unclear authority, delayed decision-making, missing insurance details, or lack of reliable location data when a traveler needs help. Vietnam’s national emergency numbers are accessible nationwide: 113 (police), 114 (fire), and 115 (ambulance/medical). For group operations, these numbers are necessary but not sufficient. They must be integrated into a corporate-grade plan that includes bilingual activation support, defined transport triggers, and a single accountable incident lead. The risk gap to manage (what can disrupt your duty-of-care posture): 1) Language - 115 operators may have limited English. A bilingual guide or 24/7 operator support should initiate the call and confirm the dispatch details. 2) Location accuracy - in dense city blocks or rural areas without clear addressing, response delays often come from unclear directions. GPS pins and landmark references should be standardized in the trip pack. 3) Traffic variability - even in cities, ambulance arrival time can be affected by traffic. Plan for alternative private transfers for low-to-medium severity cases, with pre-approved payment rules. 4) Uneven medical facility standards - private/international facilities are more likely to support English communication and faster intake, while public facilities can be slower and process-driven. The plan should specify which facilities are “default” by district and time-of-day. At evaluation stage, corporate stakeholders typically ask for proof that your supplier can execute under pressure: documented SOPs, a 24/7 escalation line, and incident documentation. If you need a reference point for execution proof, see why partners choose Dong DMC and our partner success stories. Use the framework below to define what is mandatory vs. optional when building Vietnam emergency protocols for tour groups. This structure helps procurement compare suppliers consistently and gives HR a clear basis for risk acceptance. Mandatory (minimum acceptance criteria): - 24/7 emergency hotline with named escalation owners and response expectations (SLA). - Medical emergency SOP covering: assess, call, evacuate, admit, follow-up - including documentation steps and communication cadence. - Insurance mandate including emergency treatment + evacuation/medevac + repatriation, with verifiable proof collected pre-trip. Many corporate programs set a minimum evacuation/medevac threshold of USD 100,000+ depending on policy. - Hospital access plan (by city and by region) with at least one private/international option and one public fallback, plus after-hours intake expectations. - Audit trail artifacts: incident log template, approvals workflow, expense tracking method, and data retention rules. Optional upgrades (justify based on itinerary risk): - Enhanced staffing (example: 2 guides for rural days or multi-coach splits) to reduce single-point-of-failure risk. - Remote activity rescue capability for trekking, caving, boat-based, or highland segments where ambulance access may be delayed. - Traveler tracking and alerting integration with corporate tools (or agreed operational substitute such as scheduled check-ins, geofenced venues, and roll-call audits). Supplier acceptance checklist (use in RFP scoring): - Can the supplier demonstrate a scalable incident model (minor to major) and explain who takes command? - Can they provide sample anonymized incident reports with timestamps, decisions, approvals, and receipts? - Do they commit to brand-protected execution (white-label, partner-first communications), protecting your company’s internal and external reputational risk? City-based MICE (Hanoi, HCMC, Da Nang): emergency response is generally faster due to hospital density and urban access. Planning priority: traffic timing, venue egress points, and clear “who decides” escalation. Incentives with offsites (coastal, highlands, CSR field days): emergency planning should include pre-mapped routes to the nearest suitable facility, defined thresholds for ambulance vs. private transfer, and a buffer strategy. Bleisure add-ons (small groups splitting from main program): duty of care risk increases due to dispersion. Planning priority: traveler tracking or check-in rules, simplified emergency cards, and clear rules for “if you’re separated from the group.” A medical emergency plan should be designed into the program, not added as an email attachment. For corporate groups, the plan must be easy to execute in the first five minutes and easy to audit in the following five days. Blueprint decisions to finalize before contracting: 1) Hospital mapping by hotel cluster and by venue cluster (conference venue, gala venue, offsite activity zones). 2) Transport triggers - define when the default is 115 ambulance vs. private/hotel transfer vs. specialized operator rescue (for remote segments). 3) Language support - assign who speaks Vietnamese for emergency calls and hospital intake, and what translation tools are approved. 4) Insurance workflow - how proof is collected pre-trip, where it is stored securely, and who calls the insurer. 5) Payment controls - pre-approval thresholds, method of payment (cash float, corporate card, DMC paid-and-rebilled), and receipt standards. Embedding readiness without disrupting the program: - Allocate 15-30 minutes on Day 1 for a structured safety briefing and a micro-drill: confirm emergency numbers, test the group channel, and validate that each traveler can share location. - Pin the emergency card in the group channel (and/or in the corporate trip app), including hotel address in Vietnamese and a map pin. - Assign roles: client lead, DMC incident lead, guide lead, and a back-up decision-maker if the primary contact is in transit or unavailable. Your travelers should not need to search for numbers during an incident. Store these contacts in three places: printed one-page card, pinned in the group channel, and inside your corporate trip app (if used). Vietnam emergency numbers (nationwide): - 115 - ambulance/medical emergency - 113 - police - 114 - fire Tourist support hotlines (verify before travel): - 1900 1109 and 1800 1091 are commonly cited for tourist support. Because hotline coverage can change, verify current availability for your itinerary and dates as part of your pre-departure validation. Trip Emergency Card - minimum fields (copy into your template): 1) Program name, city, dates, hotel name 2) Hotel address in Vietnamese + Google map pin link 3) Nearest landmark (e.g., “opposite [building name]”) 4) DMC 24/7 hotline (primary + secondary) 5) Client lead phone + corporate security/HR number 6) Emergency numbers: 115 / 113 / 114 7) Traveler fields (kept securely): full name, passport number, insurer name, policy number, insurer 24/7 hotline, allergies/conditions if disclosed per policy Emergency planning is partly itinerary engineering. The same medical incident can have very different outcomes depending on drive time, traffic, and venue egress. This section is written to be inserted into a proposal as “Operational Risk Controls.” Routing principles to reduce response time: - For city programs, base routing on known traffic patterns and avoid stacking tight back-to-back transfers across peak hours. Practical reference: traffic and protocol risk controls. - For rural or remote day trips, document the time-to-hospital estimate and include a fallback transport plan if ambulance access is delayed. - For higher-risk activities (trekking, remote sites), build a 2-hour buffer in the operational schedule to absorb evacuation delays without collapsing the rest of the program. Venue and hotel selection criteria (add to your sourcing checklist): - Proximity to a suitable facility (private/international where possible for English intake) - Road access quality and realistic vehicle approach points (coach access, ambulance access, security gates) - Front desk capability to coordinate transport and provide address in Vietnamese - Availability of on-call doctor services (where offered) and clarity on payment method For groups, road access is a recurring operational constraint. If your program includes multiple hotels or high coach volumes, see our hotel access and coach logistics playbook. Insurance and payment are where corporate compliance and operational reality collide. A good emergency protocol makes payment predictable and auditable. Insurance mandate (recommended minimum structure): - Emergency outpatient/inpatient treatment - Evacuation and medevac (commonly required at USD 100,000+, subject to corporate policy) - Repatriation - 24/7 insurer hotline accessible from Vietnam Proof required pre-departure (define your compliance gate): - Insurer name, policy number, coverage summary, and 24/7 emergency number - Named insured list (or confirmation method) aligned to traveler manifest - Corporate policy on pre-existing conditions disclosures (handled securely and only if required) Incidentals protocol (avoid budget surprises): Choose one method and document it: - Cash float: pre-approved USD 200 per group (or policy-defined) for small urgent payments. Require receipt photos within 30 minutes of spend. - Corporate card: define who carries it and approval rules for medical spend. - DMC paid-and-rebilled: the DMC pays locally to reduce friction, then rebills with receipts and incident log references. This supports consolidated invoicing and audit trails when implemented with strict documentation. An emergency protocol is only as strong as its first five minutes. Corporate groups require a playbook that scales from a minor incident to a major event without improvisation, and that produces documentation that procurement and HR can accept. Scalable incident model (used for staffing and escalation): - Minor: first aid, local clinic or pharmacy, minimal program impact. Managed by the guide with ops oversight and documentation. - Small/local: requires transport to hospital/ER, impacts a subset of delegates, requires client lead notification and controlled spend approvals. - Major: life-threatening event, multiple affected travelers, significant program disruption, requires full escalation: DMC management, corporate security/HR, insurer coordination, and possibly embassy notification. Authority and spend approvals (define before arrival): - Who can authorize emergency transport spend? - Who can approve hospital deposits? - Who is the single incident commander on-site? - Who communicates to corporate HQ, and how often? Below is a step-by-step SOP designed for group leaders, guides, and corporate client leads. Each step includes the documentation artifact needed for audit readiness. Step 1 - Assess (0-3 minutes) Operational actions: - Provide immediate first aid within trained scope (e.g., CPR if trained, stabilize and immobilize where appropriate). - Stop the activity and secure the area (crowd control, traffic safety). - Categorize incident: minor vs. small/local vs. major. Documentation to capture: - First timestamp: time incident identified - Symptoms observed and actions taken - Names of responders and witnesses (if applicable) Step 2 - Call (parallel actions, 1-5 minutes) Call 115 for medical emergencies. Use a Vietnamese-speaking guide or operator support to reduce miscommunication. Information to provide to 115: - Exact location: hotel name, address in Vietnamese, nearest landmark, and GPS pin - Patient details: age (approx.), gender, condition, consciousness, breathing status - Contact callback number and who will meet the ambulance Internal escalation (should happen simultaneously): - Notify DMC 24/7 ops line - Notify client lead (and corporate security/HR per agreed matrix) Documentation to capture: - Time call placed, operator details if available, and any instructions received - Screenshot/record of GPS pin sent in group channel (if policy permits) Step 3 - Evacuate (5-30+ minutes depending on context) Decision tree: - Urban (typical planning assumption): 115 ambulance with an expected response window of 8-15 minutes in many city contexts, subject to traffic. - Urban fallback / lower severity: private/hotel transfer (taxi/Grab) when clinically appropriate and approved, often faster than waiting for ambulance during peak traffic. - Rural/remote: anticipate delays. Operator rescue or pre-arranged transfers may take 30 minutes to 2+ hours depending on access. Documentation to capture: - Why the transport method was chosen (clinical and logistical rationale) - Vehicle details, driver name/plate where possible - Departure time, arrival time Step 4 - Admit (hospital intake and financial controls) Operational expectations to plan for: - Private/international hospitals are more likely to support English communication and may provide faster intake, but often require upfront payment (deposit) with later insurance reimbursement. - Public facilities may be slower and process-driven. Use as a fallback when clinically appropriate or when directed. Insurance workflow: - Notify insurer as soon as stabilized and obtain a case/reference number - Confirm whether direct billing is possible or reimbursement applies Criteria to consider for international medevac (case-dependent): - Need for specialized care not available locally - Insurer and medical provider recommendation - Typical destinations referenced in insurance pathways include regional hubs such as Bangkok or Singapore, with lead times and cost implications that must be insurer-managed Documentation to capture: - Hospital admission time, treating physician/unit, case number - Copies/photos of receipts, deposit slips, and itemized invoices - Insurer reference number and contact details Step 5 - Follow-up (audit trail and return-to-program rules) Operational actions: - Complete incident report within 12-24 hours (or per corporate policy) - Collect medical note/discharge summary where available - Decide return-to-program with documented clearance (self-declared for minor issues or medically advised for more serious cases) - Conduct a post-incident review to capture corrective actions Notification triggers (case-dependent): - Corporate security/HR escalation per policy - Embassy notification if required for lost documents, severe incidents, or insurer guidance Documentation to capture: - Full timeline log (minute-by-minute where practical) - Decision rationale and who approved spend - Corrective actions and prevention steps for the remainder of the program Staffing and redundancy: - For rural or multi-point programs, consider two guides (or guide + ops runner) to avoid single-point-of-failure if one person is managing a patient. - For large groups with split movements, designate an incident lead per sub-group and a central ops controller. Communications plan (minimum viable control): - One group channel for operational updates (WhatsApp or corporate-approved equivalent) - Escalation chain: guide - ops - client lead - corporate security/HR - Update intervals during active incidents: every 30 minutes until stable, then every 2-4 hours or per corporate policy Visibility and traveler location: If your corporate program uses traveler tracking, define how the on-ground team accesses traveler location while respecting privacy and data minimization. If you do not have a corporate tracker available for delegates, use a simpler operational substitute: - scheduled check-ins (morning, midday, end-of-day) - roll-call audit at departures/arrivals - location pin sharing rules during offsite movements For partners who require a centralized view of movements and confirmations, our Dong DMC Agent App is built for trade operations and can support operational coordination and confirmations for multi-component programs. From approximately May to October, typhoon and flood impacts are a planning consideration in parts of Vietnam. Your emergency protocol should include disruption rules, not only medical response. Controls to document for corporate approval: - Monitoring source and cadence (who checks, how often) - Pre-approved rerouting authority and spend thresholds - Minimum contingency basics for disrupted movements (example: 72-hour essentials appropriate to your group profile and venues) - Traveler accountability: check-in cadence and location confirmation during disruptions Corporate travel managers often need to report upward after programs and demonstrate control: to procurement (cost and supplier performance), to HR (duty of care), and to leadership (reputational risk management). Vietnam emergency protocols for tour groups should therefore include measurable outcomes and a standard “proof pack.” Recommended operational KPIs: - Time-to-activate: minutes from incident identification to 115 call and internal escalation - Time-to-transport: minutes to depart scene (ambulance arrival or private transfer departure) - Time-to-admit: time from departure to hospital intake - Documentation completeness: incident report + receipts + approvals present (yes/no) - Spend variance: emergency spend vs. pre-approved thresholds and reason codes - Compliance rate: percentage of travelers with verified insurance proof collected pre-trip A procurement-ready proof pack typically includes: - Emergency SOP (the auditable playbook) - Escalation matrix (names, roles, response expectations) - Hospital directory by city/region with addresses in Vietnamese and English - Training records (first aid readiness, guide briefings, role assignments) - Sample anonymized incident report with timeline log, approvals, and receipts structure If you need examples of how execution is documented across programs, see our partner success stories. These case outlines are designed for internal reporting without unnecessary detail: Urban transfer scenario: delegate illness during conference day - rapid decision to use private transfer due to traffic - admission to private ER - insurer case number recorded - delegate rejoined program with clearance. Rural stabilization scenario: incident during offsite - first aid and stabilization - transport plan activated with realistic rural timing - incident log maintained - remainder of group program continued via pre-defined continuity plan. Weather reroute scenario: storm disruption - traveler check-in executed - alternative routing approved within thresholds - consolidated invoicing with variance explanation - post-op corrective actions documented. Enhanced emergency readiness should be quoted as a transparent line item. This reduces disputes and supports procurement sign-off. Typical line items to separate: - Additional guides / on-site medical staff (if required) - Remote rescue readiness for high-risk days - Tracking and communications tooling (if provided) - Increased buffers impacting transport and staffing hours In market practice, programs with enhanced protocols and insurance add-ons can result in an estimated 5-10% uplift depending on scope and itinerary risk profile. Your procurement team can treat this as a risk-control premium with clear deliverables. This section provides replicable formats you can copy into your corporate templates. Each item is designed to support policy compliance, duty-of-care governance, and audit readiness. Policy and traveler compliance: - Traveler manifest finalized (names match passports) - Insurance proof collected for 100% of travelers (policy number + 24/7 insurer hotline) - Medical disclosures handled per company policy (secure storage, least-access principle) - Emergency contact card prepared (printed + digital pinned message) Supplier and SOP readiness: - DMC 24/7 hotline tested (call and response confirmed) - Escalation matrix approved (including after-hours) - Hospital directory validated for itinerary cities and rural extensions - Payment protocol confirmed (cash float vs. corporate card vs. DMC paid-and-rebilled) Technology and visibility: - Group channel created and pinned message published (contacts + hotel address in Vietnamese + map pin) - Location sharing method agreed (GPS pin and/or What3Words) - Traveler tracking integration confirmed (if applicable) or substitute check-in schedule defined Use this as an agenda in your welcome meeting: 1) Roles and who to call first (client lead and DMC hotline) 2) Vietnam emergency numbers: 115 (medical), 113 (police), 114 (fire) 3) How to share location (send a pin, share hotel card, use nearest landmark) 4) What to do if separated from the group (check-in rule, meeting point, channel usage) 5) Payment rules (do not pay deposits without approval unless life-threatening - follow protocol) 6) Quick verification drill (everyone sends location pin in the channel) One-page Emergency Action Plan (EAP) - recommended sections: - Emergency numbers and 24/7 hotline - Escalation matrix and update cadence - Hospital list with addresses in Vietnamese and English - Transport triggers and decision authority - Documentation checklist (incident log, receipts, approvals) Hospital directory (Excel/Sheets) - recommended columns: - City/area - Facility name (EN + VN) - Address (EN + VN) - Phone number - Estimated drive time from hotel cluster - English support likelihood (yes/no/unknown) - Payment expectations (deposit likely, card acceptance notes) Incident report (PDF or form) - required fields: - Incident type and severity classification - Location (address + GPS pin) - Timeline (time stamps for each action) - People involved and notified (with times) - Decisions and rationale - Costs and receipts (itemized) - Outcome and return-to-program status - Corrective actions and prevention notes RACI chart (crisis roles) - suggested roles: - Responsible: Guide lead, DMC incident lead - Accountable: Client lead / corporate travel manager (as defined) - Consulted: Corporate security/HR, insurer - Informed: Procurement (post-incident), leadership (as required) To maintain budget control during emergencies, document thresholds and tie every expense to an incident reference code. Recommended structure: - Define pre-approved categories: transport to hospital, medical deposits, interpreter support, replacement transport for the group - Set spend thresholds: example USD X per incident without additional approval; above that requires named approver - Require receipts and timestamps for each line item - Use consolidated invoicing with an appendix: incident summary + receipts bundle + approvals trail If your organization evaluates suppliers on sustainability and governance, you can also reference our sustainable operations policy as part of supplier documentation. Q: What are Vietnam’s emergency numbers and which one is ambulance? A: Vietnam’s national emergency numbers are 113 (police), 114 (fire), and 115 (ambulance/medical). For corporate groups, plan that a Vietnamese-speaking guide or a 24/7 operator support line initiates the 115 call to reduce language risk. Q: What response times should we assume for urban vs. rural incidents? A: For planning, many city contexts use an expected ambulance response window of 8-15 minutes, while rural and remote areas can extend to 30 minutes to 2+ hours depending on access. For remote days (trekking, highlands, boat activities), build 2-hour operational buffers and document fallback transport methods. Q: Can our travelers access English-speaking hospitals in Vietnam? A: Private/international hospitals in major cities are more likely to have English-speaking staff and faster intake. Public facilities can be slower and process-driven. For compliance and traveler experience, map at least one private/international option per city cluster, and document payment expectations (often upfront deposit) and reimbursement workflow. Q: How do we ensure cost control if a private hospital requests upfront payment? A: Pre-define a payment protocol: who can approve deposits, what spend thresholds apply, and whether payment is via cash float, corporate card, or DMC paid-and-rebilled. Require itemized receipts and tie each expense to an incident reference code for consolidated invoicing and audit trails. Q: How do we ensure auditability after an incident? A: Require an incident pack with (1) timeline log with timestamps, (2) decision rationale and approver names, (3) communications record (who was notified and when), (4) receipts and itemized invoices, (5) insurer case/reference number, and (6) corrective actions documented post-incident. This structure supports HR duty-of-care review and procurement supplier scorecards. Q: What minimum insurance should we mandate for Vietnam corporate programs? A: Mandate coverage for emergency treatment plus evacuation/medevac and repatriation. Many corporate programs require USD 100,000+ evacuation/medevac coverage, subject to your internal policy. Collect proof pre-departure (policy number and 24/7 insurer hotline) and store it securely with access control. Q: How do we locate travelers quickly during disruptions or medical events? A: Use a controlled communications plan: a single group channel, scheduled check-ins, and standardized location sharing (GPS pins and/or What3Words). For corporate systems, align with your traveler tracking tool if available and define what the on-ground team can access while respecting privacy and data minimization. Q: Do we need to verify tourist support hotlines before travel? A: Yes. Tourist support numbers such as 1900 1109 and 1800 1091 are commonly cited, but hotline coverage and routing can change. As part of your pre-departure checklist, validate current functionality for your travel dates and cities and document the verification timestamp. If you are evaluating Vietnam for an upcoming corporate program, request our itinerary-specific Emergency SOP + Hospital Access Pack (Hanoi, HCMC, Da Nang, plus rural extensions). It includes an escalation matrix, a hospital directory format, and a sample anonymized incident report structure to support procurement and HR approval. Fast quotations. Brand-protected operations. Zero missed arrivals. Emergency numbers (113/114/115) and planning context are widely referenced across Vietnam tourism safety guidance and operator protocols. For corporate duty of care, validate critical hotline availability and hospital access assumptions during your pre-departure check for each program. Commonly referenced sources used for this operational summary: - Vietnam safety and emergency guidance: https://visitvietnam.org.vn/en/safety - Emergency number references and traveler guidance (cross-checked): https://viet10travel.com/dealing-with-emergencies-in-vietnam-a-tourists-guide/ and https://sungetawaystravel.com/vietnam-medical-emergency/ - Operator-tier emergency response concepts and rural timing realities (adventure context): https://oxalisadventure.com/emergency-response-procedure-in-oxalis-adventure-tour/ - MICE unforeseen event management context: https://trusteddmc.com/news/1570-unforeseen-event-management-and-emergency-protocols-for-micebleisure-groups-in-vietnam.aspx - US State Department advisory reference point (Level can change): https://travel.state.gov/content/travel/en/traveladvisories/traveladvisories/vietnam-travel-advisory.html
Planning Takeaways
1) Why Vietnam emergency protocols matter for corporate groups (duty of care, control, and audit readiness)
1.1 Decision framework for procurement and HR approval
1.2 Setting expectations by program type (MICE vs. incentives vs. bleisure add-ons)
2) Building a medical emergency plan into the program design (planner-ready blueprint)
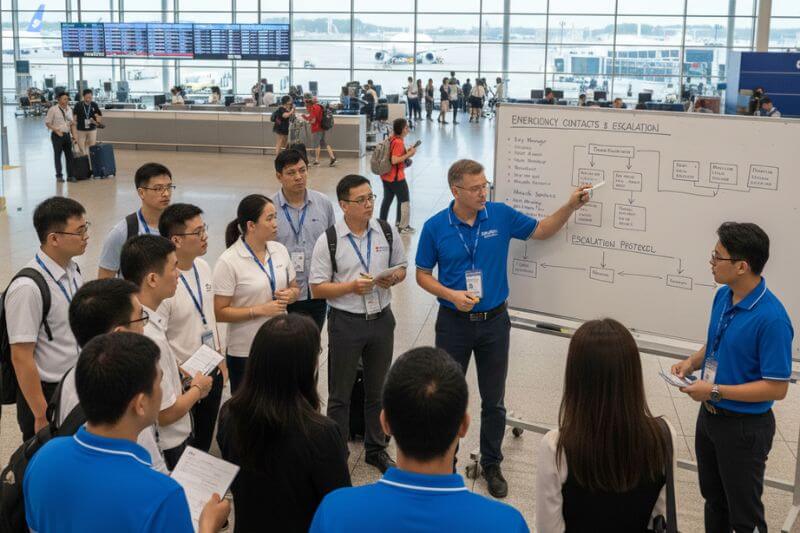
2.1 Essential emergency contacts and what to store in your corporate trip pack
2.2 Itinerary engineering: buffers, routing, and venue/hotel selection for faster care
2.3 Insurance and payment readiness (compliance and cost control)
3) Operational considerations: running medical incidents smoothly on the ground

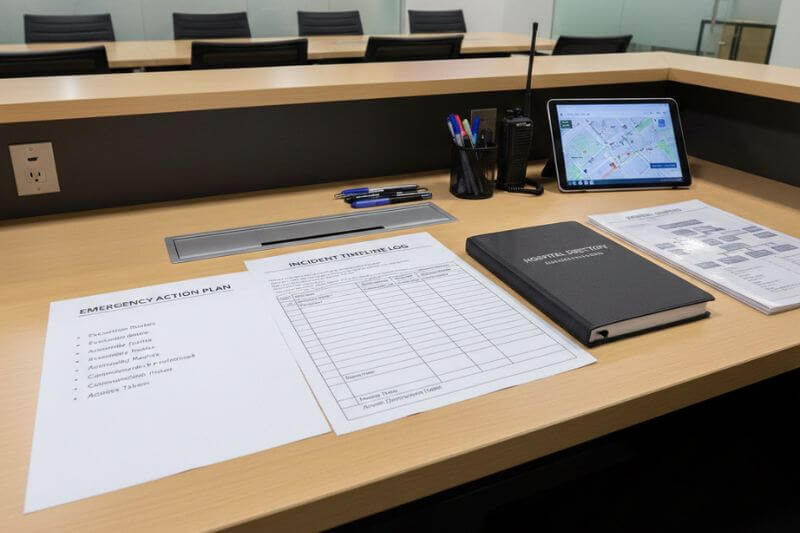
3.1 Ground SOP (medical): an auditable playbook you can attach to your proposal
3.2 Staffing, communications, and visibility controls (what corporate managers should require)
3.3 Weather and disruption risk controls (May to October planning considerations)
4) Demonstrating control to stakeholders: metrics, proof pack, and safe case storylines
4.1 KPIs you can report (supplier scorecards and post-program reviews)
4.2 Proof pack (what to request from your Vietnam ground operator)
4.3 Safe case storylines you can use internally (non-sensational, governance-focused)
4.4 Commercial structure that prevents hidden costs (how to package enhanced protocols)
5) Tools and checklists (implementation assets for corporate teams)
5.1 Pre-trip compliance checklist (copy/paste)
5.2 Day-1 briefing run-of-show (15-30 minutes)
5.3 Templates (formats to request from your DMC)
5.4 Budget-control tools: pre-approval thresholds and consolidated invoicing
Frequently Asked Questions (Corporate Travel Managers)
Talk to a Market Specialist (Vietnam Emergency SOP + Hospital Access Pack)
Sources and verification notes (for 2026 planning files)
 EN
EN



